COM research team’s study improves outcomes for patients undergoing chest wall surgery
A faculty member and group of students from the University of New England College of Osteopathic Medicine (UNE COM) published a study earlier this year whose findings may help relieve pain in pediatric patients following surgery to the chest.
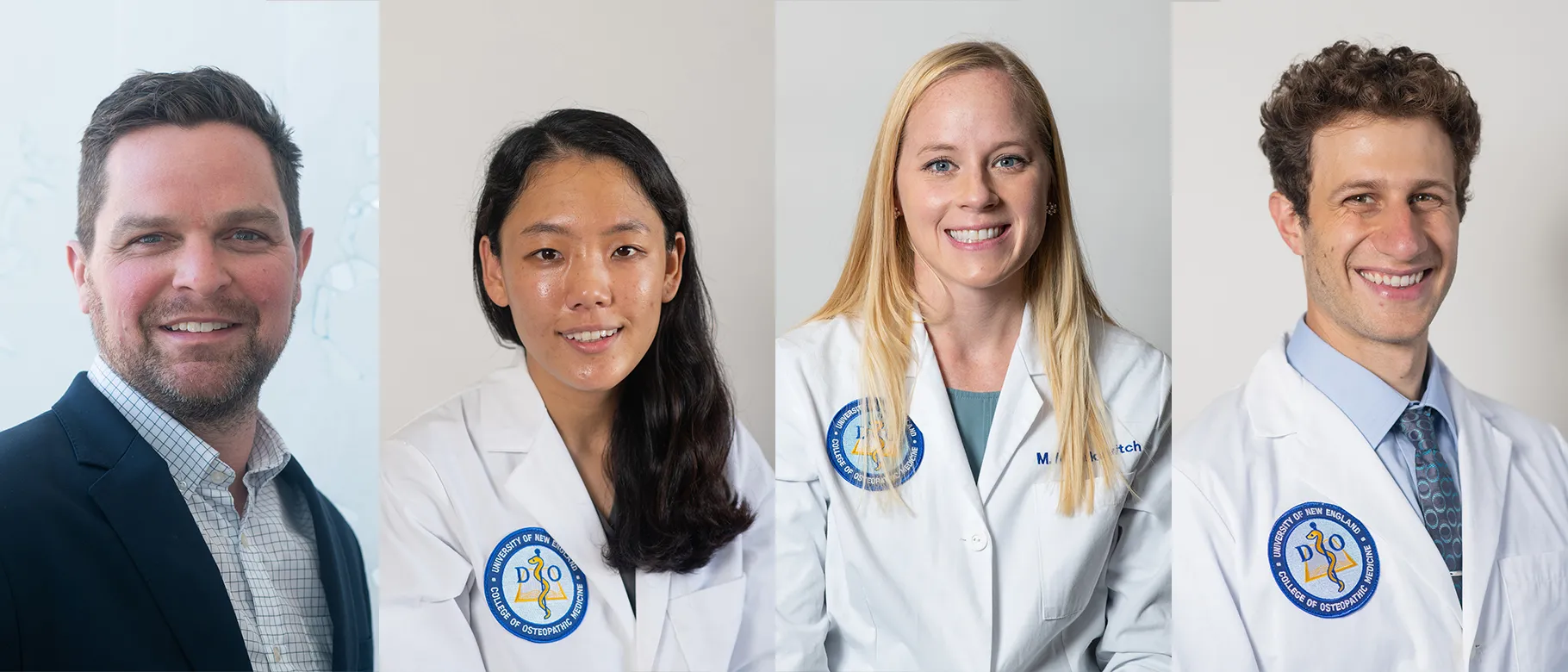
Joel Talsma, M.S., assistant clinical professor in the Department of Biomedical Sciences, is lead author on the study, “Forgotten Branch of the Intercostal Nerve: Implication for Cryoablation Nerve Block for Pectus Excavatum Repair,” along with students Melanie Kusakavitch (D.O., ’24), Dawon Lee (D.O., 25), and Christoph Niederhauser (D.O., ’25) in collaboration with researchers from the University of California San Francisco (UCSF).
In the study, recently published in the Journal of Pediatric Surgery, the researchers examined methods for reducing patient pain following surgery to repair pectus excavatum, a deformity in the chest wall that causes a depression in the middle of the chest. The condition rarely requires treatment, but severe cases may compress the heart and lungs and require surgical correction.
According to Talsma, children who undergo surgery to correct pectus excavatum often report high levels of pain post-operation — a finding noted by Sunghoon Kim, M.D., a pediatric surgeon at UCSF Benioff Children’s Hospitals who specializes in repairing chest wall malformations and is one of the study’s authors.
Kim reached out to Talsma to help refine his use of cryoablation — a technique he uses to ease patients’ pain by using a cold probe to numb the primary nerve along the ribs, known as the main intercostal nerve.
However, Talsma said, the procedure only helps with pain for a limited amount of time.
He and his team set out to map the intercostal nerves with the goal of identifying new targets for cryoablation that may reduce pain for longer periods of time. Using cadavers, Talmsa and his team identified a co-lateral branch of the intercostal nerve they suspected would be a good target for additional cryoablation therapy.
The team reported their findings to Kim, who has integrated the branch into his approach and vastly reduced average pain scores post-surgery. Using this data, the researchers concluded that cryoablation of the intercostal nerve and its co-lateral branches improves pain control after surgery to repair pectus excavatum.
According to Talsma, the study was a great way for his students to immerse themselves in, and contribute to, the anatomical literature he said is often overlooked as part of a student’s early medical education.
“A lot of time, anatomy is discounted in pre-clinical medical education, but not at UNE,” he remarked. “This study was a good way for our students to understand how anatomy matters and translates into a clinical procedure with real, patient-centered implications.”
UNE recently launched a Master of Science in Clinical Anatomy degree program, as well as a post-baccalaureate certificate in clinical anatomy, through the College of Osteopathic Medicine intended to bolster the workforces in medical education and clinical research.
Talsma added that research on the intercostal nerve is limited, and the study serves as an early introduction to the peer-review process that students will encounter as they progress through medical school, residency, and their careers as physicians and medical researchers.
“I think it was great for them to get through that review process and learn how to carry out a project from start to finish,” he said.