Medical student draws praise for developing 3D-printed pelvic model to improve anatomical understanding

University of New England College of Osteopathic Medicine student Sarah Swanick (D.O., ’28) spent four months last semester creating a 3D-printed anatomical model of the pelvis, lumbar spine, and femur — not for a class or research project, but purely to understand pelvic anatomy more deeply.
The end result: Her 3D-printed pelvic model will be featured in the December issue of the Journal of Osteopathic Medicine after placing second in a national student competition at the American Osteopathic Association's Osteopathic Medical Education Conference, held in September in Nashville, Tennessee.
But Swanick said the greatest impact of the passion project at UNE’s medical school was the heightened understanding of anatomy the model lent her and many others. Medical school professors both at UNE and beyond asked her to share the model or present it to their classes.
The third-year medical student, who graduated from UNE with a degree in medical biology in 2023, began the project in January after encountering several clinical situations that made her want to satisfy her curiosity about how ligaments work.
“In a clinic shift, we had a patient who had a very interesting pelvis pain and one of my professors — Dr. (Kiran) Mangalam (D.O.) — explained how (the photos of) ligaments that we see in textbooks aren’t actually correct, they actually wrap all the way around the bone,” Swanick said. “So that made me think, ‘I don't know anything about this, and it seems super clinically relevant. I want to learn more about ligament attachments and see how they move.’”
Working over four months on her own time between classes and while studying for board exams, Swanick found 3D-printable anatomy files on Thingiverse and combined multiple models to create what she needed. She worked with Sophia Crockett-Current, manager of UNE's P.D. Merrill Makerspace on the Biddeford Campus, to print the components, visiting the makerspace 19 times between January and April.
"She's like, ‘I don't understand what the books are saying. I don't understand what these pictures are showing me. I want to understand what's going on, and so I need to just be able to see it happen,’" Crockett-Current recalled.
The real challenge came in making the model functional. That led Swanick to seek out other mentors to help explain how the ligaments attach to the pelvis to ensure anatomical accuracy.
Assistant Professor Tyler Redway, Ph.D., sat down with Swanick and went through every ligament in the pelvis and helped her understand how pelvic ligaments attach.
Assistant Clinical Professors Jay Roop, D.O., provided guidance on construction techniques and adhesives and Stuart Damon, D.O., suggested using exercise bands to represent ligaments, a stroke of innovative brilliance that led Swanick to use the brown bands from her own physical therapy exercises for a lower back injury.
“The pelvis is such a dynamic part of the skeleton, yet it’s so often shown as a solid, immovable structure—especially in most anatomical models,” Redway said. “Sarah was on a mission to better understand the more intricate movements of the pelvis and their connections to the vertebral column and femur.”
At the national conference in Nashville in September, Swanick’s poster presentation about her pelvic model drew praise from faculty and physicians. Professors from other osteopathic schools, such as the New York College of Osteopathic Medicine, requested information about replicating the project, Swanick said.
Her professors at UNE’s medical school, which is Maine’s only medical school, called her quest a combination of creativity, resourcefulness, anatomical precision, and unwavering persistence.
Assistant Clinical Professor Lynette Bassett, D.O., encouraged Swanick to bring the model to a medicine training workshop in the Massachusetts Berkshire Mountains, where physicians who had authored medical textbooks praised her work. Mangalam asked Swanick to present the model during a class on physiologic changes during pregnancy.
“Sarah’s passion for the project was palpable whenever we spoke about it,” said Redway, whose research focuses on anatomy education programs for high schools. “The final product was a detailed, functional pelvic model that not only highlighted the anatomical relationships among the sacrum, innominate (hip bone), and femur, but also allowed for demonstration of their key joint movements.”
Swanick is currently completing her clinical rotations at MaineGeneral in Augusta before she plans to take a year off to serve as a teaching fellow with UNE Professor Frank Willard, Ph.D., before graduating in 2028.

Swanick, shown above on rotation at MaineGeneral, made the model in her free time.
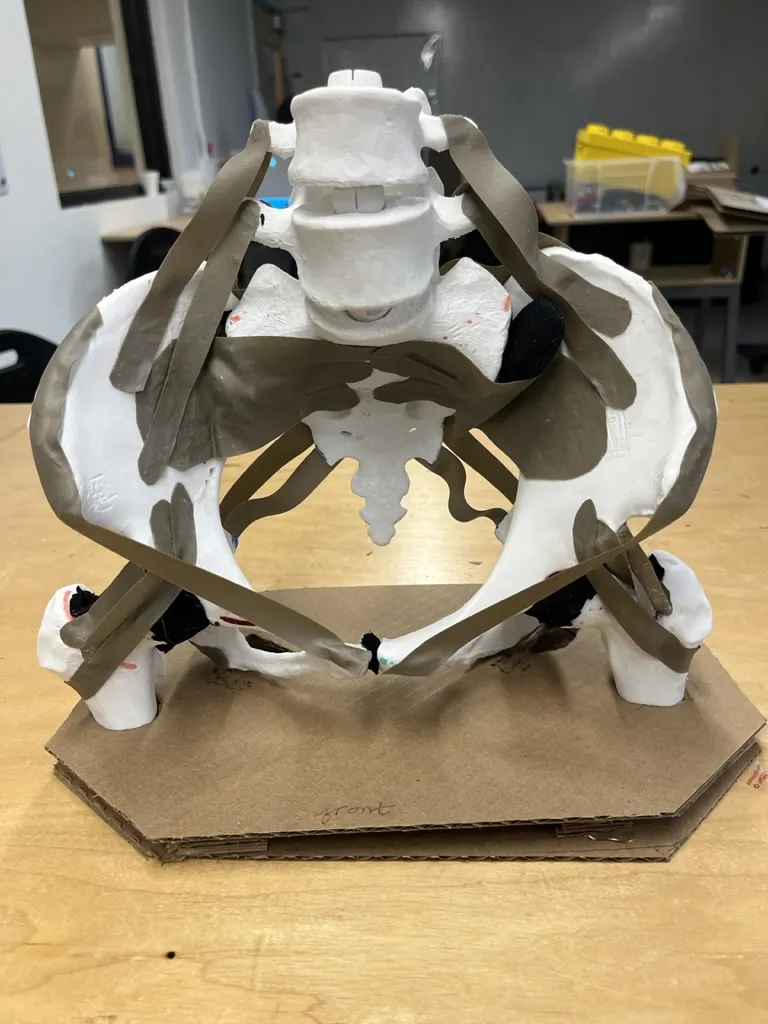
Swanick used physical therapy bands for ligaments.